Diabetic retinopathy is the most common cause of vision loss among people with diabetes and the leading cause of blindness among working-age adults. It's a significant health challenge, with over a third of people with diabetes developing some signs of diabetic retinopathy. With the right knowledge about causes, symptoms, diagnosis, and treatment options, we can better manage diabetic retinopathy.
Causes and Risk Factors of Diabetic Retinopathy
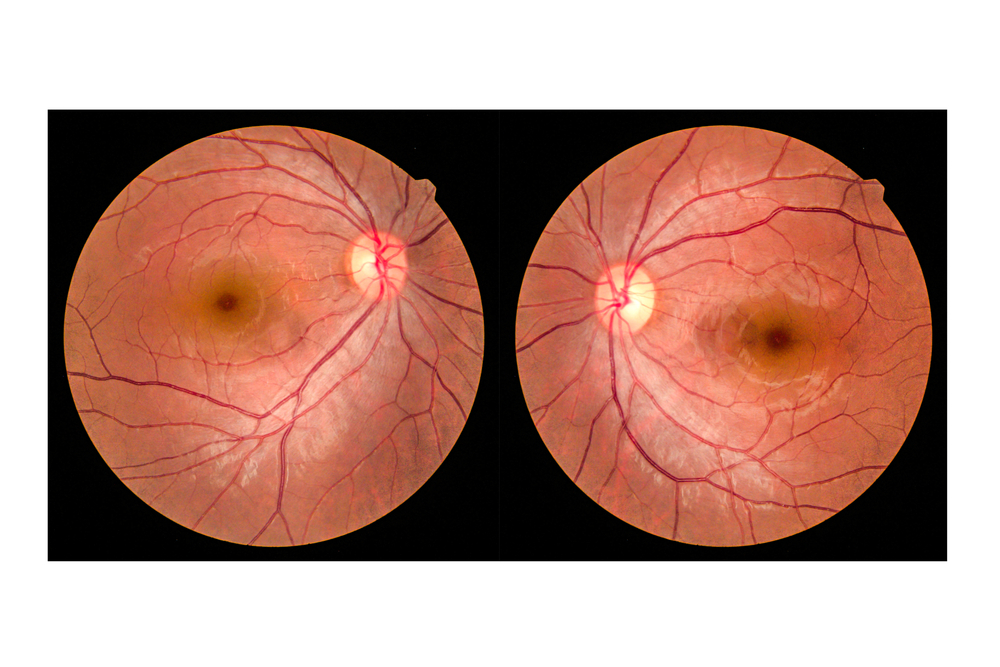
Diabetic retinopathy occurs when there's damage to the blood vessels in the tissue at the back of the eye. Poorly controlled blood sugar is a risk factor, as it can accelerate the onset and progression of diabetic retinopathy.
Individuals with type 1 and type 2 diabetes are at risk for this condition. However, the longer someone has had diabetes, the more likely they are to develop diabetic retinopathy. Other risk factors include high blood pressure, high cholesterol, tobacco use, being pregnant, or being of African or Hispanic heritage.
Recognizing the Symptoms
Recognizing the symptoms of diabetic retinopathy can be tricky because it often starts without any noticeable vision problems. That's why regular check-ups are so important. However, as the condition progresses, several symptoms might become apparent. These can include fluctuating vision, blurred or distorted vision, dark or empty areas in your vision, or experiencing floaters—tiny specks or dots that float in your vision.
You may also notice that colors appear faded or washed out. In severe cases, diabetic retinopathy can lead to vision loss. It's important to remember that experiencing any of these symptoms doesn't automatically mean you have diabetic retinopathy, but they should be taken seriously. If you experience any of these symptoms, seek medical attention immediately.
Importance of Early Diagnosis
Early diagnosis in diabetic retinopathy is crucial. Since the condition often begins without symptoms, regular eye exams are necessary, especially for individuals with diabetes. A comprehensive eye exam can help detect diabetic retinopathy before you start noticing any symptoms, allowing for earlier treatment and a better prognosis.
The American Diabetes Association recommends that people with type 1 diabetes have their first eye exam within five years of their diabetes diagnosis and that people with type 2 diabetes have an eye exam immediately after diagnosis. After that, most people with diabetes should have an eye exam every year.
Early detection and treatment can reduce the risk of blindness by 95 percent. It's a compelling reason to ensure you're keeping up with your eye health, particularly if you have diabetes or are at risk.
What Are the Treatment Options?
There are several treatment options available. The best treatment for you will depend on the specifics of your condition, but they all aim to prevent, slow, or stop the progression of diabetic retinopathy.
In the early stages, good blood sugar control can usually slow the progression. As the condition advances, treatments may include medication injected into the eyes, laser treatment, or surgical procedures. Early detection is key, and while these treatments can be highly effective, they work best when diabetic retinopathy is found early in its course.
Conclusion
If you or a loved one has diabetes, make sure you're taking the necessary steps to monitor your eye health. Regular eye exams, maintaining control of your blood sugar levels, and understanding the risk factors for diabetic retinopathy are all essential.
To learn more on diagnosing and treating diabetic retinopathy, visit Manheim Family Eye Care at our office in Manheim, Pennsylvania. Please call (717) 423-8400 to schedule an appointment today.








